A First—But Not Last—for Cancer Care in Sierra Leone
Posted on Jan 21, 2020

This time two years ago, Margaret had never heard of choriocarcinoma—cancer of the cervix and uterus. So when clinicians at Koidu Government Hospital (KGH), the Partners In Health-supported facility in Kono, Sierra Leone, diagnosed her with it in July 2018, she remembers feeling a wave of fearful confusion.
“I had no idea what was happening,” Margaret said. “None of my family or friends has had this sickness before. My mum thought I was going to die when they explained to her that it was cancer. When people in Sierra Leone have cancer, they rarely survive.”
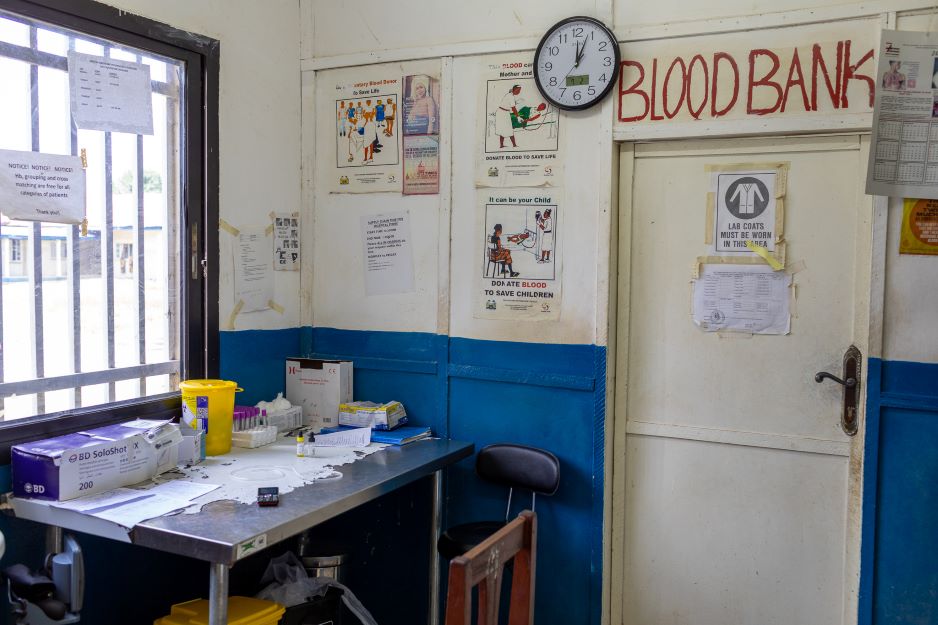
Indeed, Margaret’s health was dire when she was readmitted at KGH in July 2018, five months after initially being treated at the hospital for a molar pregnancy (commonly a precursor to choriocarcinoma). Experiencing a fever and intense bleeding to the point of unconsciousness, Margaret was unable to walk, stand, or eat, and relied on the hospital’s blood bank and emergency blood donations from family members and KGH staff to stay alive.
“She bled two or three times a day. We needed to constantly replace her blood,” KGH midwife C.J. said. “Even maternal staff on the ward thought she might not make it.”
Clinicians had quickly discovered the cause of Margaret’s condition—a carcinoma, or cancerous growth, located in her cervix. After getting her bleeding under control, the KGH team turned to the larger problem: How could they treat this case, in a country where oncology care is nearly nonexistent?
“Very challenging” was how Dr. Marta Lado, chief medical officer for PIH-Sierra Leone, diplomatically described the current state of cancer care in Sierra Leone, where even basic health infrastructure is limited, at best. In partnership with the Ministry of Health, PIH is adding high-quality cancer care to its work strengthening Sierra Leone’s health care system, and is beginning to tackle the many challenges the country faces when it comes to oncology.
First of all, the diagnostic process is long and expensive, as samples and lab tests need to be sent to external private laboratories for analysis. If the result is cancer, a limited number of oncology drugs are available; Sierra Leone has no established national chemotherapy program. What’s more, most patients arrive at health facilities when their cancer is already advanced to a stage where palliative care is the only viable option, having held off going to see a doctor for fear of the cost of care and lack of access to nearby clinics or hospitals.
Another concern is that nurses and pharmacists don’t have formal training opportunities in cancer care, so many lack expertise in how to manipulate and administer oncology drugs. The country also has limited lab capabilities to properly diagnose cancer, and social support programs—which would help patients meet such needs as food, transportation, and housing—are rarely part of care.
All of these programs and resources are currently being planned for at KGH, which each month sees one or two patients arriving with any type of cancer—usually advanced stage lymphoma, leukemia, or, as in Margaret’s case, choriocarcinoma.
“At KGH, when we find a case that is an early stage and can benefit from treatment, we have been able to refer patients to PIH in Rwanda, or buy some chemo and administer it locally with the collaboration of a clinic in Freetown that has some trained and skilled staff,” Lado explained. “But honestly, these are very exceptional cases. We strongly believe that as we grow in our clinical care, we will start identifying more cancer cases in early stages; therefore, we need to start organizing the necessary care for them at KGH.”

Margaret was one of these exceptional cases—and one who helped set in motion the expansion of cancer care at KGH.
PIH-Sierra Leone’s supply chain team managed to secure a shipment of Methotrexate, the drug that could cure Margaret, from India. She began inpatient chemotherapy in August 2018, and by December was discharged, needing to come back to the hospital every three to four weeks for her next round of treatment.
“Margaret looks great now and is a joy to have around the ward,” said Isata Dumbuya, KGH’s maternity manager, last summer. “She likes making everyone laugh and is always trying to help with things.”
After a year of care, in August 2019, Margaret completed her full course of treatment, with the next step involving quarterly blood tests to monitor her health. Now, she is poised to become the first woman to survive chroriocarcinoma at KGH.
She won’t be the last, however. Because her case made Methotrexate available, two other women with choriocarcinoma are currently receiving treatment.
More patients will follow, Lado said. “At KGH we are working really hard to increase the standard of care for our patients, including setting up a basic protocol for chemotherapy. We have already started with choriocarcinoma, and care for Kaposi Sarcoma and some types of lymphomas in children will be developed this year.”

The aim too is to expand this care beyond KGH. “The government of Sierra Leone is extremely supportive with our programs and excited about all of our initiatives in Kono. Together, we are setting examples and role modelling, to give hope for a better health care system in the entire country,” Lado said.
At the center of this slow and steady progress at KGH and throughout Sierra Leone is Margaret. “She really has carved a path for others needing this care,” Dumbuya said.
Margaret herself may someday be providing it, as her experience as a patient has informed her future career goals. Determined to become a nurse, Margaret has returned to school with support from PIH, and on any given day can often be found in the KGH maternity ward offering moral support to patients.
“The doctors and nurses were encouraging, and my mum sees me now and she has good faith,” she said. “I want to get a job so I can be working and supporting my parents—I want to be a nurse. I like it at the ward; I want to be part of the KGH midwife team.”

